By: Lola Aquilar
Gout is a type of inflammatory arthritis that can cause significant pain and other complications. It often occurs in one joint at a time (such as the big toe joint). It may get worse or flare at times, and there may be no symptoms at all when it is in remission. When gout is chronic, it can lead to gouty arthritis, which is a form of arthritis that gets worse over time. While there is no cure for gout, it can be treated and managed with medication and at-home management strategies.
Symptoms of Gout
If your big toe joint suddenly begin hurting, gout may be a potential diagnosis. However, there are many other signs and symptoms of gout.
Gout flares may start suddenly without any seeming cause. They can last days or weeks. Flares are often followed by weeks, months or years of remission with no symptoms. While the big toe joint is the most common joint that displays symptoms, other common affected areas include lesser toe joints, knees and ankles.
Some common symptoms of gout include:
- Intense pain
- Redness
- Heat
- Swelling
Gout may be diagnosed through a physical examination, X-rays and lab tests. Gout can only be diagnosed during a flare when signs and symptoms are evident in a joint and when lab tests have a positive result.
What Is the Cause of Gout?
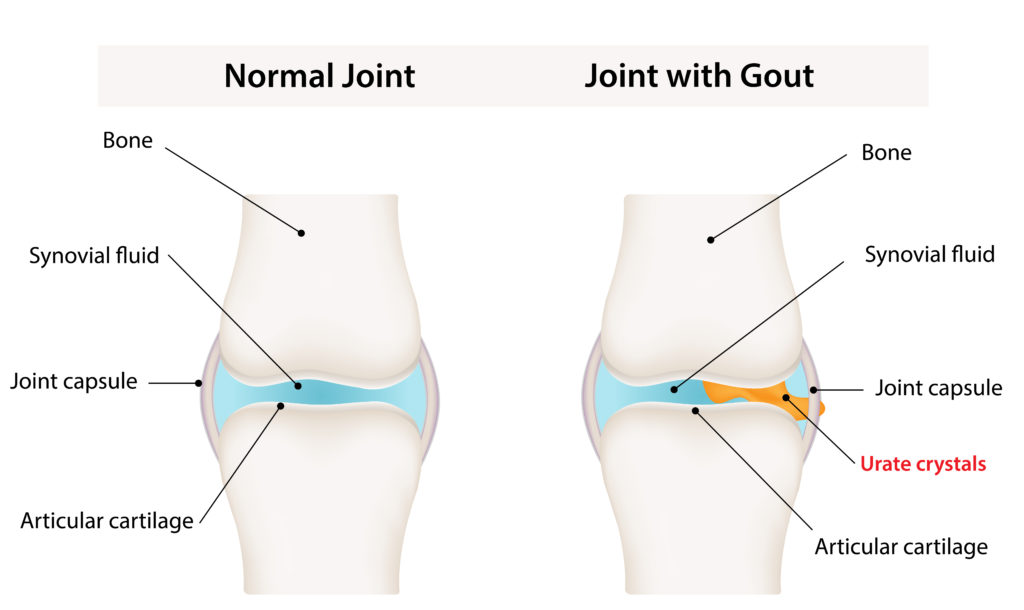
Gout is the result of a condition called hyperuricemia; wherein there is too much uric acid in the body. Uric acid is produced in the body as purines are broken down. Those purines may be found in your body naturally or in the foods you eat. When too much uric acid is in the body, uric acid crystals (monosodium urate) can become built up in the body tissues, joints and fluids. Hyperuricemia may not always cause gout, and it does not need to be treated unless gout occurs.
Gout is more common for people who:
- Are male
- Are obese
- Have congestive heart failure, hypertension, insulin resistance or diabetes, metabolic syndrome or poor kidney function
- Use diuretics (water pills)
- Drink alcohol
- Eat or drink foods containing high fructose levels
- Have a diet high in purines, such as red meat organ meat and certain seafood
Treatments for Gout
Doctors who specialize in gout are called “rheumatologists.” Once a rheumatologist makes a diagnosis, your primary care physician can manage the condition.
Treatment for gout typically involves nonsteroidal anti-inflammatory drugs (NSAIDs) like steroids, ibuprofen and drugs like colchicine. However, prevention of gout and future flares is a primary focus of treatment.
Preventing Gout and Gout Flares
If you are at risk for gout or you have already been diagnosed with gout, there are strategies you can take to prevent flares.
- Maintain a healthy weight
- Limit alcohol
- Eat less purine-rich foods
- Stop medications associated with hyperuricemia (like diuretics)
- Eat a healthy diet low in fructose
- Engage in low-impact physical activity
- Protect your joints from injuries
You can also prevent tophi and kidney stones that often result from chronically high levels of uric acid. Tophi are hard deposits of uric acid under the skin. Preventative medications to lower uric acid levels may include drugs like pegloticase, febuxostat and allopurinol.
How to Live with Gout
Although gout can be debilitating, it can be managed to prevent flares. You should work with your doctor to prevent flares, and if you do experience pain and other symptoms, seek medical treatment right away.
If you are diagnosed with gout, there is no cure. However, it is possible to live without frequent flareups that significantly impact your life. Gout prevention is the best policy.








Leave A Comment